Fentanyl overdoses in our community: What you can do
On April 14, 2016 the B.C. Ministry of Health announced the number of drug-related overdoses in the province had become a public health emergency, citing 474 preventable overdose deaths in British Columbia in 2015.
In the six months that followed, they collected more data about overdoses (both fatal and non-fatal) and tried to proactively warn people about risks. During that same period, hundreds more died of illicit drug overdoses – 622 in the first 10 months of 2016, with at least 60 per cent of those directly linked to fentanyl.
It is tragically clear that this response has been insufficient and ineffective. In my next MLA Report I’d like to detail some of the recommendations made by the UVic Centre for Addictions Research of B.C. on how the province can better respond to this crisis.
But to start, I think it is important to highlight the local resources available to support drug users and their loved ones, and what to do if someone is overdosing. I would like to extend my most sincere gratitude to those constituents who have reached out to teach me about this emergency and share memories of their loved ones who have been lost to this tragic epidemic. Fentanyl-related overdoses are happening all over the province, and our riding is no exception.
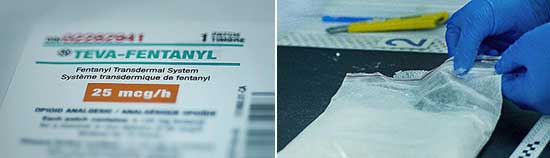
Fentanyl is a synthetic opioid that is cheap and can be cut into other drugs like cocaine, crack, MDMA (ecstasy), crystal meth, heroin, fake oxy, and fake Percocet without the user knowing. Fentanyl is 50 to 100 times more toxic than morphine, making it horribly easy to accidentally overdose on. Carfentanil, recently detected in Vancouver, is 100 times more potent than fentanyl and can be fatal to humans in 20 microgram doses – smaller than a grain of salt.
Opioid overdose symptoms include: the person not being able to stay awake, talk or walk; slow or no pulse; slow or no breathing; gurgling; skin looks pale or blue and feels cold; pupils are pinned or eyes rolled back; the person could be vomiting and their body may be limp.
Naloxone, a medication that can reverse the effects of an opioid overdose when injected into an arm, buttocks or thigh muscle, can reverse slowed breathing in one to five minutes. It is now widely available without a prescription around the province and is credited with saving countless lives. In most naloxone kits there is also a face shield that can be used for administering rescue breathing (as in CPR).
If someone is experiencing an opioid overdose you should: stimulate the person to see if they are unresponsive; call 911 and tell them if the person is not breathing; clear the person’s airway and provide rescue breathing (one breath every five seconds). Use one injection of naloxone if it is available, monitoring the person to see if they will need another dose. Be aware that an overdose can return and additional naloxone may be necessary. When paramedics arrive tell them as much as you can about the drugs used and doses.
Training and naloxone kits are available across B.C. To find a site near you, visit Toward the Heart or call 811 any time day or night. In the Oak Bay – Gordon Head riding kits are available at some pharmacies and: Royal Jubilee Hospital Prescriptions (DT 1200 – 1952 Bay St.), Royal Jubilee Hospital – Emergency Department (1952 Bay St.), and Victoria Mental Health Centre (2328 Trent St.).
For substance user services and support call Island Health at 250-213-4444 or the 24-hour crisis line at 1-888-494-3888.
Comments are closed.