MLA Report: Fentanyl crisis shows need for comprehensive, proactive approach
As I sat down to write this article, with a dozen tabs open to fentanyl-related stories and studies, a new headline made its way to the front page and it hit me like a tonne of bricks. “Overdose deaths involving fentanyl fill Vancouver morgues to capacity.” One life lost is heartbreaking; the scale of this emergency can hardly be articulated in a way that respects and represents the grief felt around B.C.
The situation in Vancouver is particularly dire, but fentanyl-related overdoses are happening all over the province and our riding is no exception. The reach and magnitude of this crisis has been tragic. The fact that it has only continued to escalate since the B.C. Ministry of Health declared it a public health emergency on April 14 is horrific in its own right.
Also in the news at the time of writing is an article in the Vancouver Sun that reads “the B.C. government is almost doubling its advertising spending [to $15 million] five months before the provincial election, but the minister responsible says it’s to raise awareness of the fentanyl overdose crisis…”
People are dying. We need to help them, not make ads about them.
In 2009 when H1N1 hit B.C., the province put $80 million towards fighting the flu that killed 57 people. Illicit drug overdoses have killed 622 people in the first 10 months of this year, surpassing car crash fatalities to become the leading non-natural cause of death in B.C.
By their own, arguably generous, estimate the provincial government has spent $15 million to prevent and respond to overdoses. Yet even their plan to create 500 new addiction treatment spaces by 2017, a promise made by the premier in the 2013 election, remains unmet. So far only 220 new spaces have become available. And during the same period, the number of substance-abuse treatment beds for young people has dropped 25 per cent to just 89.
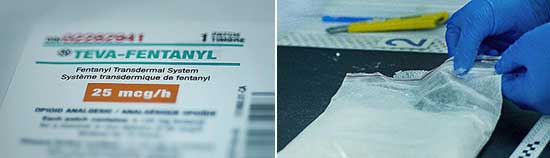
The government’s resources thus far have largely been focused on collecting data and distributing naloxone kits, a medication that can reverse the effects of an opioid overdose. They are important initiatives, to be sure, but they are reactionary. They kick in when someone is already in the throes of an overdose. If we want to get ahead of this crisis, we need to step in with a comprehensive plan to support people before they are that close to dying.
Reports released by researchers with the University of Victoria’s Centre for Addictions Research of B.C. (CARBC) provide evidence of the inadequacy of government responses to this emergency, but they also detail a path forward.
For Victoria specifically, they write that by delaying the implementation of supervised consumption services – despite the indications of a growing overdose epidemic and widespread reports of washrooms in social service agencies being used as unofficial and unsupervised injection sites – the province is ignoring the evidence.
As Dr. Bruce Wallace and Dr. Bernie Pauly, researchers at CARBC and faculty members at UVic, wrote in the Globe and Mail, “What is needed is a more comprehensive approach.
“This should include supervised consumption as well as increased access to treatment and opiate-substitution therapy. There is a wealth of evidence that supports the effectiveness of supervised consumption services in preventing overdoses, preventing the transmission of blood-borne disease and increasing access to referrals to treatment and opiate substation therapy.”
Last week Island Health finished the public consultation phase of their application to open a supervised consumption site in Victoria. I hope you will join me in imploring the provincial government to do everything in its jurisdictional power to support this process along, as well as follow CARBC’s recommendations to increase the number addiction-treatment facilities.
Comments are closed.