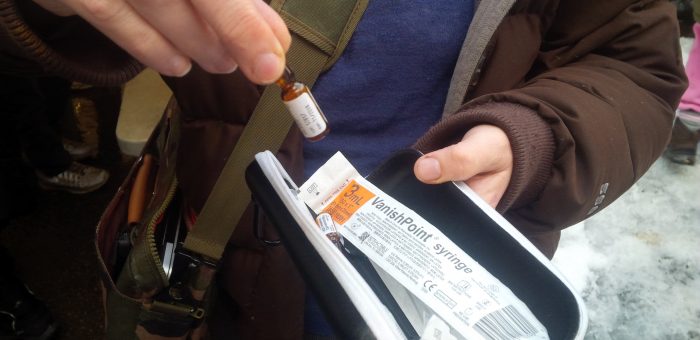
VANCOUVER B.C. – B.C. Green Party leader Andrew Weaver and New Westminster candidate Jonina Campbell released the following statements after touring a pop-up safe injection site near East Hastings and Columbia streets in Vancouver:
“I have been deeply moved by the dedication and commitment of those working at Vancouver’s pop-up safe injection sites – volunteers who are working with few resources to save lives that would otherwise likely be lost,” Weaver said. “Sarah Blyth, Anne Livingston and others who have acted so selflessly are to be commended for taking action in an incredibly desperate situation.
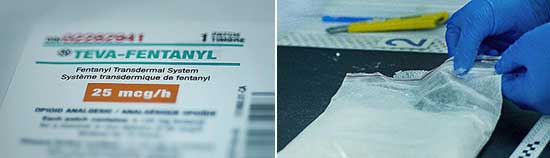
“Today, the B.C. Coroners Service reported that a staggering 755 people died from illicit drug use from January 1 to November 30 this year. The opioid crisis is out of control. Federal Health Minister Jane Philpott needs to immediately declare a national health emergency, which would give chief medical officers the power to deal with this crisis as a health issue. It is also critical that the federal government immediately repeal aspects of the Harper-era Bill C-2 that make it extremely difficult for cities to open safe-injection facilities like Vancouver’s InSite. Community members have been forced to pull together scarce resources to provide life-saving services on their own. It is unconscionable that our communities are barred from responding with the most effective, life-saving measures. The consequences are simple – the more we dither, the more people die.”
“The approach of the past, to treat drug use as a criminal issue, does not work. Drug use is a public health issue. Lack of treatment facilities has been a major contributing factor, while the systematic underfunding of mental health services has had broad reaching consequences. The scale of this tragedy forces us to ask some very difficult questions, including the question of decriminalizing illicit drugs. The Portugal model, where use or possession of illicit drugs was changed from a criminal to administrative offence, has proven to dramatically reduce STIs and drug-related deaths. These deaths can happen to anyone. As a society, we must respond accordingly.”
“I would like to call on all provincial leaders to come together on this issue,” Campbell added. “Andrew is the only party leader to tour a pop-up safe-injection site. While Premier Clark and John Horgan have stated that they will not visit one, I urge them to reconsider. We must put humanity above all else. The fentanyl crisis is a community health issue and therefore, local politicians must learn firsthand about what is occurring and what can be done to stop these tragic deaths.”
“We must not forget our responsibility to support first responders, frontline workers and volunteers, who are trying to cope with insufficient resources and the trauma of being on the ground. This is a grassroots effort of downtown eastside community members who have come together, because it is their friends and family who are suffering and dying. What I witnessed today was a tragedy of epic proportions. Few British Columbians understand the scale of what is happening. We must support those who put themselves in the middle of it, hoping to save one life at a time.”
– 30 –
Media contact
Mat Wright, Press Secretary, Office of Andrew Weaver, MLA
+1 250-216-3382 | mat.wright@leg.bc.ca